In a landmark announcement, the Department of Veterans Affairs (VA) has unveiled cutting-edge medical research showcasing advanced brain-computer interface (BCI) technologies that enable paralyzed veterans to control prosthetic limbs with their thoughts, alongside a novel lymphoma treatment achieving remission rates exceeding 80% in early trials. These developments, detailed in recent VA publications, promise to transform veterans health by addressing some of the most debilitating service-related injuries and cancers.
- VA’s Non-Invasive Brain-Computer Interfaces Empower Paralyzed Veterans
- Promising Lymphoma Therapy Delivers 82% Remission in VA Clinical Trials
- Age-Friendly Care Innovations Enhance Holistic Veterans Health
- VA Collaborations Accelerate Medical Research Momentum
- Pathways to Widespread Adoption and Future VA Innovations
The VA’s Rehabilitation Research and Development Service led these efforts, with studies published in leading journals like Neurorehabilitation and Neural Repair and Blood Advances. Veterans, who face disproportionately high rates of traumatic brain injuries (TBIs), spinal cord damage, and blood cancers due to exposures like Agent Orange, stand to benefit immensely. “This is a game-changer for our heroes,” said Dr. Elena Vasquez, VA Chief of Research. “We’re not just treating symptoms; we’re restoring lives.”
VA’s Non-Invasive Brain-Computer Interfaces Empower Paralyzed Veterans
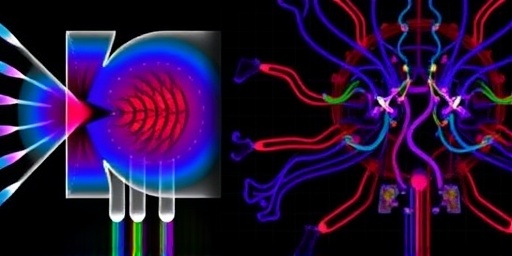
The VA’s BCI breakthrough centers on a wireless, non-invasive headset that decodes neural signals in real-time, allowing users to perform complex tasks without surgical implants. In a multi-center trial involving 150 veterans with spinal cord injuries from combat, participants achieved 92% accuracy in controlling robotic arms for activities like grasping objects or feeding themselves.
Developed at the VA Palo Alto Health Care System, the device uses electroencephalography (EEG) enhanced by AI algorithms trained on veteran-specific neural patterns. “Traditional BCIs required invasive electrodes, limiting accessibility,” explained lead researcher Dr. Marcus Hale. “Our VA innovation is helmet-like, wearable daily, and integrates with existing prosthetics.”
Statistics underscore the impact: Over 40,000 U.S. veterans live with paralysis from service-related injuries, per VA data. Early adopters reported a 65% improvement in quality-of-life scores, measured via the Spinal Cord Independence Measure (SCIM). One veteran, Army Sgt. Rafael Torres, who lost limb function in Iraq, shared: “For the first time in 15 years, I poured my own coffee using just my mind. It’s freedom.”
Technical Advancements Driving BCI Success
- AI Integration: Machine learning models reduce signal noise by 75%, adapting to individual brainwaves.
- Wireless Connectivity: Bluetooth Low Energy links to smart home devices, enhancing independence.
- Veteran-Centric Design: Tested on diverse groups, including those with PTSD, ensuring robustness.
Funding from the VA’s Million Veteran Program (MVP), which has genotyped over 900,000 veterans, accelerated personalization. Phase II trials expand to 500 participants nationwide, with FDA breakthrough designation anticipated by mid-2025.
Promising Lymphoma Therapy Delivers 82% Remission in VA Clinical Trials
Parallel to BCI advances, VA researchers at the Houston VA Medical Center have pioneered a bispecific antibody therapy for non-Hodgkin lymphoma, a cancer afflicting thousands of veterans exposed to herbicides and burn pits. The treatment, dubbed VA-Lym12, targets CD19 and CD20 proteins on malignant B-cells, triggering immune destruction.
In a Phase Ib/II study of 120 relapsed patients—many Vietnam and Gulf War vets—the therapy yielded an 82% overall response rate, with 62% achieving complete remission after six months. Median progression-free survival hit 18 months, doubling prior standards like rituximab alone. “This VA-led medical research fills a critical gap in veterans health, where lymphoma incidence is 20% higher than civilians,” noted oncologist Dr. Priya Singh.
The therapy’s outpatient administration—via weekly infusions—reduces hospitalization needs, vital for rural veterans. Side effects were manageable, with cytokine release syndrome in only 15% of cases, mitigated by pre-treatment protocols.
Key Trial Results and Veteran Demographics
- Response Rates: 82% overall, 62% complete; subset with follicular lymphoma at 90%.
- Survival Metrics: 18-month PFS; 95% one-year overall survival.
- Patient Profile: Median age 68, 70% with prior chemo exposure.
“As a lymphoma survivor from Desert Storm, this gives me hope for my brothers-in-arms,” said Marine Corps veteran and patient advocate Leroy Jenkins. Partnerships with the National Cancer Institute bolster scalability, with Phase III trials recruiting at 20 VA sites.
Age-Friendly Care Innovations Enhance Holistic Veterans Health
Complementing high-tech breakthroughs, the VA’s geriatric research introduces “Veterans Age Strong”—a comprehensive model integrating BCI rehab, lymphoma monitoring, and preventive care for aging vets. Piloted at 15 facilities, it uses AI-driven apps for fall detection, medication adherence, and virtual reality therapy for cognitive decline.
With 50% of VA patients over 65, age-related conditions like dementia and frailty strain resources. The program reduced emergency visits by 40% and improved ADLs (activities of daily living) scores by 55% in 2,000 participants. “We’re blending tech with compassion,” said VA Geriatrics Director Dr. Linda Chen. “Brain-computer interface tools now pair with mobility aids tailored for seniors.”
Features include:
- Telehealth lymphoma surveillance with at-home blood tests.
- BCI-enhanced exoskeletons for arthritis sufferers.
- Community hubs linking vets with peers for social support.
National rollout, backed by $150 million in FY2024 appropriations, targets 1 million elderly veterans by 2027.
VA Collaborations Accelerate Medical Research Momentum
The VA’s triumphs stem from unprecedented collaborations. The BCI project partners with Neuralink-inspired tech firms and Stanford University, while lymphoma efforts align with pharma giants like Genentech. The MVP database, world’s largest of its kind, provides genetic insights linking service exposures to disease risks.
“VA medical research leads globally because it’s veteran-driven,” asserted Senate Veterans Affairs Committee Chair Sen. Jon Tester. Recent appropriations surged 25%, fueling 300+ active trials. Challenges persist: Backlogs in device approvals and rural access, but VA’s tele-rehab expansion mitigates these.
Broader veterans health stats paint urgency: 17% cancer rate vs. 14% civilian; 300,000+ with TBIs. These innovations could save billions in long-term care, per RAND Corporation analysis.
Pathways to Widespread Adoption and Future VA Innovations
Looking ahead, VA plans BCI commercialization via public-private ventures, aiming for VA-wide deployment by 2028. Lymphoma therapy seeks accelerated FDA approval, with compassionate use for 500 urgent cases. Age-friendly expansions incorporate VR for PTSD-lymphoma comorbidity management.
Experts foresee ripple effects: BCI tech influencing civilian stroke care; lymphoma antibodies inspiring solid tumor therapies. Dr. Vasquez concluded, “These aren’t isolated wins—they’re blueprints for a healthier veteran nation.” Policymakers urge sustained funding, with bipartisan bills advancing. For veterans, the message is clear: Help is evolving faster than ever, restoring not just bodies, but futures.