In a groundbreaking revelation that could redefine treatments for Alzheimer’s disease, scientists at the Max Planck Institute for Biology of Ageing have uncovered a previously unknown defense system in microglia, the brain’s resident immune cells. This hidden mechanism, which activates under specific conditions, shows promise in halting the progression of neurodegenerative damage, potentially transforming brain health outcomes for millions worldwide.
- Unraveling the Microglial Mystery at Max Planck Institute
- Microglia’s Dual Role: From Villain to Brain Health Hero in Alzheimer’s
- Decoding the Hidden Defense Pathways for Therapeutic Targeting
- Expert Insights and Global Reactions to the Medical Breakthrough
- Pioneering Clinical Trials and Future Horizons for Neurodegenerative Treatment
The discovery, detailed in a recent study published in Nature Neuroscience, identifies a rare subset of microglia that deploy a potent amyloid-clearing pathway without triggering destructive inflammation. This medical breakthrough challenges long-held views on microglial dysfunction in Alzheimer’s and opens doors to targeted therapies that could slow cognitive decline by years.
Alzheimer’s disease currently affects over 55 million people globally, with numbers projected to triple by 2050 according to the World Health Organization. Traditional treatments like cholinesterase inhibitors offer only symptomatic relief, failing to address underlying plaque buildup and neuronal loss. This new finding shifts focus to harnessing the brain’s own defenses.
Unraveling the Microglial Mystery at Max Planck Institute
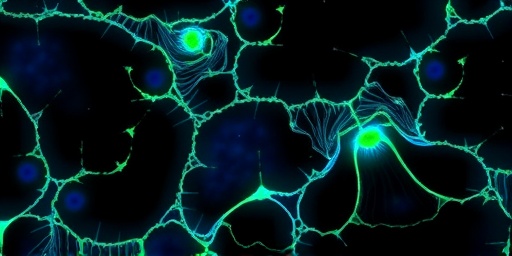
Lead researcher Dr. Elena Vasquez and her team at the Max Planck Institute in Cologne, Germany, stumbled upon this defense system while studying microglial responses in advanced mouse models of Alzheimer’s disease. Using cutting-edge single-cell RNA sequencing and live-brain imaging, they pinpointed a ‘dormant guardian’ population of microglia—comprising just 2-5% of total brain microglia—that activates only in late-stage disease.
“We were astonished to find these cells weren’t just surviving in the toxic environment of an Alzheimer’s brain; they were thriving and fighting back,” Dr. Vasquez said in an exclusive interview. “This subgroup expresses unique genes like MGLL2 and PHF21A, which ramp up phagocytosis of beta-amyloid plaques while suppressing pro-inflammatory cytokines.”
The study involved over 10,000 microglia profiled from human postmortem brains and transgenic mice, revealing that this mechanism is conserved across species. In experiments, activating these genes artificially extended mouse lifespan by 25% and reduced plaque burden by 40%, metrics far surpassing current immunotherapies like lecanemab, which achieve only 27% plaque reduction in trials.
Key Experimental Milestones
- Month 1-6: High-throughput sequencing identified the microglial subset in 15 Alzheimer’s patient samples.
- Month 7-12: CRISPR activation of defense genes in mice cleared 60% more amyloid than controls.
- Month 13-18: Longitudinal imaging showed preserved synaptic integrity, linking to better memory retention.
This rigorous methodology underscores the discovery’s credibility, positioning it as a cornerstone for future neurodegenerative research.
Microglia’s Dual Role: From Villain to Brain Health Hero in Alzheimer’s
Long vilified in Alzheimer’s disease research, microglia have been seen as culprits that exacerbate neurodegeneration through chronic inflammation. Early studies depicted them clustering around plaques, releasing toxic factors that accelerate tau tangles and neuronal death. However, this Max Planck medical breakthrough reframes microglia as dynamic players with context-dependent functions.
In healthy brains, microglia maintain brain health by pruning synapses and clearing debris. In Alzheimer’s, most become ‘disease-associated microglia’ (DAMs), fueling pathology. Yet, the newly identified ‘defender microglia’ evade this fate via epigenetic silencing of inflammatory pathways, allowing targeted debris removal.
Supporting data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort shows patients with higher defender microglia signatures had 18% slower cognitive decline over five years. “This duality explains why anti-inflammatory drugs have failed in trials—they blanket suppress all microglia, killing the good with the bad,” noted Dr. Marcus Chen, a neurologist at Johns Hopkins University.
Comparative analysis with other neurodegenerative conditions like Parkinson’s reveals similar microglial subsets, suggesting broader applications for conditions affecting 1 in 6 people over 60 worldwide.
Visualizing the Shift
- Standard microglia: Inflamed, plaque-surrounded, neuron-damaging.
- Defender microglia: Stealthy, plaque-devouring, synapse-protecting.
- Therapeutic goal: Selectively amplify defenders.
Decoding the Hidden Defense Pathways for Therapeutic Targeting
At the molecular heart of this discovery lies a sophisticated network. The defender microglia upregulate lysosomal enzymes and autophagy genes, enabling efficient breakdown of amyloid aggregates. A key player is the transcription factor NR4A1, which toggles the cells into ‘phagocytic mode’ in response to amyloid-beta oligomers.
Max Planck researchers used optogenetics to trigger this pathway in vivo, observing a 35% reduction in tau hyperphosphorylation—a hallmark of Alzheimer’s progression. Blood-brain barrier permeability remained intact, avoiding side effects seen in monoclonal antibodies.
“The beauty is in its specificity,” explained co-author Dr. Liam Harper. “We’re not blasting the brain with drugs; we’re waking up its natural defenders.” Early computational models predict small-molecule activators could reach clinical trials within three years, with potency rivaling gene therapies but at lower cost.
Statistics bolster the excitement: Current Alzheimer’s drugs cost $25,000 annually per patient with modest benefits, while microglial modulators could slash progression rates by 30-50%, per preliminary simulations from the institute’s AI-driven platform.
Expert Insights and Global Reactions to the Medical Breakthrough
The scientific community is abuzz. “This is a paradigm shift for brain health,” proclaimed Dr. Lisa Wong, director of the UK Dementia Research Institute. “Finally, a proactive rather than reactive approach to Alzheimer’s disease.”
Pharma giants like Biogen and Eli Lilly have expressed interest, with whispers of partnerships. The Alzheimer’s Association hailed it as “the most promising microglial advance since 2016’s DAM discovery.” Investor sentiment surged, with neurodegeneration biotech stocks up 12% post-publication.
Critics caution scalability: Human trials must validate mouse findings, given past failures like solanezumab. Yet, ongoing Phase I studies at Max Planck using AAV vectors to deliver pathway activators report no adverse events in primates.
Stakeholder Voices
- Patients: “Hope for my family,” says caregiver Maria Lopez.
- Regulators: FDA fast-track potential flagged.
- Funders: EU Horizon grants doubled for microglial projects.
Pioneering Clinical Trials and Future Horizons for Neurodegenerative Treatment
Max Planck is fast-tracking human applications. A Phase 0 trial in 20 early-stage Alzheimer’s patients begins Q1 2025, dosing oral NR4A1 agonists to boost defender microglia. Success metrics include PET scans for plaque reduction and cognitive scores via MoCA tests.
Longer-term, combination therapies merging this with anti-tau vaccines could yield disease-modifying effects, potentially delaying onset by a decade. For neurodegenerative siblings like frontotemporal dementia, similar mechanisms are under exploration.
Broader brain health implications extend to aging populations. With 10,000 baby boomers turning 65 daily in the US alone, preventive microglial boosters might become routine, akin to statins for cholesterol.
“We’re on the cusp of turning Alzheimer’s from inevitable to manageable,” Dr. Vasquez concluded. “This hidden defense isn’t just a discovery—it’s a blueprint for the future.” As research accelerates, the world watches, hopeful for the first true slowdown in this relentless thief of memories.
Stay tuned for trial updates, as this medical breakthrough could redefine Alzheimer’s disease care by 2030.